Pancreatic Cancer Symptoms
Pancreatic cancer symptoms do not usually appear until the disease has progressed.
They could include:
- Backache caused by abdominal pain.
- Appetite loss or unintentional weight.
- Yellowing of the skin and eye whites (jaundice).
- Stools in light colours.
- Dark urine.
- Skin itch.
- Diabetes diagnosis or existing diabetes that is becoming
more difficult to control.
- Clots in the blood
- Fatigue
Pancreatic Cancer Causes
It is unknown what causes pancreatic cancer. Doctors have identified some risk factors for
this type of cancer, such as smoking and having certain inherited gene mutations.
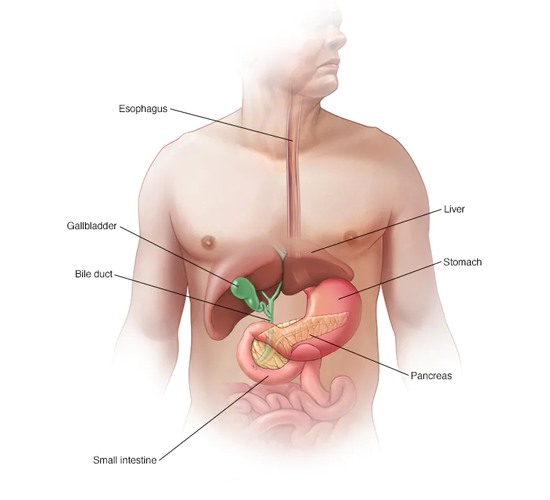
Knowing about your pancreas
Your pancreas is approximately 6 inches (15 centimetres) long and resembles a pear lying on
its side. It secretes hormones, including insulin, to assist your body in processing sugar
from the foods you eat. It also produces digestive juices to assist your body in digesting
food and absorbing nutrients.
How Pancreatic Cancer Develops
Pancreatic cancer develops when cells in your pancreas undergo DNA mutations. A cell's DNA
contains the instructions that tell the cell what to do. These mutations instruct the cells
to grow uncontrollably and to live after normal cells would have died. These accumulating
cells have the potential to form a tumour. Pancreatic cancer cells can spread to nearby
organs and blood vessels, as well as distant parts of the body, if left untreated.
Best Pancreatic Cancer Doctor in Delhi
The majority of pancreatic cancers begin in the cells that line the pancreatic ducts. This is
known as pancreatic adenocarcinoma or pancreatic exocrine cancer. Cancer can form in the
pancreas' hormone-producing cells or neuroendocrine cells less frequently. These cancers are
known as pancreatic neuroendocrine tumours, islet cell tumours, or pancreatic endocrine
tumours.
Risk elements
The following factors may increase your risk of pancreatic cancer:
- Smoking
- Diabetes
- Chronic pancreatic inflammation (pancreatitis)
- Family history of cancer-related genetic syndromes, such
as a BRCA2 gene mutation, Lynch syndrome, and familial atypical mole-malignant melanoma
(FAMMM) syndrome
- Pancreatic cancer in the family
- Obesity
- Older age, as the majority of people are diagnosed after
the age of 65.
- A large study found that the combination of smoking,
long-standing diabetes, and a poor diet increases the risk of pancreatic cancer more
than any of these factors alone.
Complications
As pancreatic cancer advances, it can lead to complications such as:
Loss of weight - Weight loss in people with pancreatic cancer can be caused
by a variety of factors. Weight loss may occur as a result of the cancer consuming the
body's energy. Cancer treatments may cause nausea and vomiting, or a tumour pressing on your
stomach, making it difficult to eat. Alternatively, your body may struggle to process
nutrients from food because your pancreas isn't producing enough digestive juices.
Jaundice - Jaundice can be caused by pancreatic cancer that blocks the bile
duct of the liver. Yellow skin and eyes, dark urine, and pale stools are all symptoms.
Jaundice is usually accompanied by abdominal pain.
Your doctor may recommend inserting a plastic or metal tube (stent) into the bile duct to
keep it open. This is accomplished through the use of a procedure known as endoscopic
retrograde cholangiopancreatography (ERCP). ERCP involves passing an endoscope down your
throat, through your stomach, and into the upper part of your small intestine. The dye is
then injected into the pancreatic and bile ducts via a small hollow tube (catheter) inserted
through the endoscope. Finally, images of the ducts are taken.
Abdomen Pain - A growing tumour may press on nerves in your abdomen,
causing severe pain. Pain relievers can make you feel more at ease. Radiation and
chemotherapy treatments, for example, may help slow tumour growth and provide some pain
relief.
Obstruction of the bowel - Pancreatic cancer that spreads to or presses on
the first part of the small intestine (duodenum) can obstruct the passage of digested food
from the stomach into the intestines.
Your doctor may advise you to have a tube (stent) placed in your small intestine to keep it
open. In some cases, surgery to insert a temporary feeding tube or connect your stomach to a
lower point in your intestines that isn't blocked by cancer may be necessary.
Prevention
You can lower your risk of pancreatic cancer by doing the following:
Quit smoking - Make an effort to quit smoking if you smoke.. Consult your
doctor about quitting methods such as support groups, medications, and nicotine replacement
therapy.
Keep a healthy weight - Maintain your current weight if you are at a healthy
weight. If you need to lose weight, aim for a gradual, consistent loss of 0.5 to 1 kilogram
per week. To lose weight, combine daily exercise with a diet rich in vegetables, fruit, and
whole grains in smaller portions.
Your risk of cancer -
If you have a family history of pancreatic cancer, you should consult with a genetic
counsellor. He or she can go over your family health history Choose a nutritious diet
Pancreatic Cancer Treatment
Treatment for pancreatic cancer is determined by the cancer's stage and location, as well as your overall health and personal preferences. When possible, the first goal of pancreatic cancer treatment for most people is to eliminate the cancer. When that isn't an option, the emphasis may shift to improving your quality of life and preventing the cancer from spreading or causing further harm.
It is possible to use surgery, radiation, chemotherapy, or a combination of these treatments. When pancreatic cancer has advanced to the point where these treatments are unlikely to help, your doctor will focus on symptom relief (palliative care) to keep you as comfortable as possible for as long as possible.
Pancreatic Cancer Surgery -
Pancreatic cancer patients may undergo the following operations:
Surgery for pancreatic head tumours - If your cancer is in the head of the pancreas, you may want to consider a Whipple procedure (pancreaticoduodenectomy).
The Whipple procedure - The Whipple procedure involves removing the head of the pancreas, the first part of the small intestine (duodenum), the gallbladder, a portion of the bile duct, and nearby lymph nodes. In some cases, a portion of the stomach and colon may also be removed.Your surgeon reconnects the remaining parts of your pancreas, stomach, and intestines to allow you to digest food
Surgery for pancreatic body and tail tumours.
Distal pancreatectomy is the surgical removal of the pancreas's left side (body and tail). Your spleen may also need to be removed by your surgeon.
The pancreas is surgically removed - In some cases, the entire pancreas must be removed. This is known as a total pancreatectomy. You can live a relatively normal life without a pancreas, but you will require insulin and enzyme replacement for the rest of your life.
Tumors affecting nearby blood vessels may require surgery. Many people with advanced pancreatic cancer who have tumours that involve nearby blood vessels are not considered candidates for the Whipple procedure or other pancreatic surgeries. Surgeons at highly specialised and experienced medical centres may perform pancreatic surgery operations such as removing and reconstructing affected blood vessels.